How Do We Stop the Opioid Epidemic Immediately? We Make These 4 Changes
The world is run by people who show up and speak up.
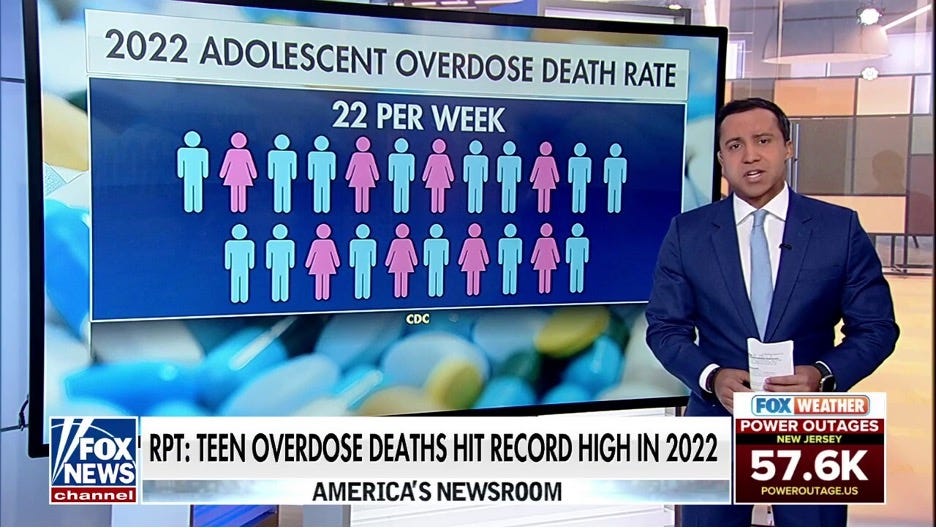
We lose 357 Americans to opioid overdose deaths every day. That is roughly one large jumbo jet, or 15 preventable deaths per hour. Can you imagine if we had one large plane full of Americans crashing and dying daily? The FAA would shut down aviation immediately until we isolated the cause and corrected it. If it’s predictable, it’s preventable. Opioid overdose deaths are both predictable and preventable. And yet our broken pathways for treatment in the American medical system approach remains largely unchanged. Last week, the deputy director of the DEA, Ann Milgram, stated, “The Opioid Epidemic has gone from being one of the many threats to American lives to the single greatest threat of our lifetime.”
Despite this bleak outlook, there is hope. There are a few simple changes we can make that would reverse this troubling trajectory and save lives overnight. These changes reduce existing artificial barriers to care and making drug use less deadly.
4. DEA: Change Suboxone from a Schedule III to a Schedule IV (non-controlled) medication
In the wake of the opioid settlements, many large pharmacy chains enacted strict internal policies to reduce the dispensing of opioid pain medications. Unfortunately, because Suboxone is also classified as a schedule three controlled substance, it is subject to the same internal pharmacy scrutiny as medications like Dilaudid, Fentanyl, and Oxycontin. Erring on the side of caution, many busy pharmacists these days simply refuse to fill it. But unlike opioids, Suboxone is a life-saving medication that reduces the chances of dying from fentanyl by 50%. It quite literally doubles your chance of survival. I talk with large chain retail pharmacists daily who tell me, “I can’t fill your prescription. It is a controlled substance.” If the DEA simply changed Suboxone’s categorization from a schedule 3 controlled substance to a schedule 4 non-controlled substance, this would disentangle Suboxone from the strict opioid pharmacy dispensing protocols, immediately increasing access to this life-saving medication to millions of Americans.
3. FDA: Change the FDA approved age range for Suboxone and Methadone from 18 and above to 14 and above
With the rise of fentanyl and xylazine-laced fentanyl, I’ve sadly seen several 14-, 15-, and 16-year-old patients who needed Suboxone. By the time these patients saw me, they were opioid dependent and had suffered multiple near fatal overdoses. In almost every case, these patients and their families saw at least ten doctors prior to me who, despite their troubling histories and very high risk of death, refused to start them on Suboxone. The refusal reason each time was “This medicine is only FDA approved for those 18 years and older.” On the first return appointment after a Suboxone initiation, one 17-year-old girl’s mother cried, saying, “You don’t know how grateful we are to have our daughter back. She went from failing grades back to being an A-B student within one week of starting Suboxone. She failed 11th grade last year because of the opioid problems. We just wish we found you sooner.” I was the 8th physician this family had seen. It took them almost a year to find me. The seven others refused to start her on Suboxone because she was under 18. This should never happen. The scientific evidence and data is irrefutable: Suboxone saves lives- no matter if you are 76 or 16. We don’t need further time or studies in teenagers to prove that. With over 300 deaths daily, our young people don’t have the luxury of time.
2. Congress: Pass the “Modernizing Opioid Treatment Access Act” (MOTA) bill to allow Addiction Psychiatrists to prescribe Methadone outside of an OBOT
Suboxone’s older cousin, Methadone, is another critical medication that prevents overdoses and saves lives. Despite being just as effective as Suboxone, it isn’t used nearly as much as Suboxone. (I’ve basically written it off.) Why? Because it is much more difficult for patients to access and remains largely uncovered by payors. Under current law, if Methadone is being prescribed for addiction, it must be prescribed and dispensed by an Office-Based Opioid Treatment Program (OBOT). These are free-standing, for profit Methadone clinics that require patients to come to the clinic every day between 5am-10am to take their daily dose of Methadone (and also charge them a fee). They also require counseling. Most of these clinics do not take any form of insurance, leaving patients with expensive daily out of pocket costs anywhere between $20-$50 dollars daily. Finally, many are in dangerous areas of town. In the DC area where I live, 2 of the 3 local Methadone clinics are in areas where I would never venture alone during the daytime.
The MOTA act would allow board certified Addiction Psychiatrists or Addiction Medicine Physicians to prescribe Methadone through regular outpatient appointments like every other medicine, immediately removing all the artificial barriers listed above and lowering overdose rates. This is a life-saving medicine that can be safely prescribed by a specialist. Right now, most people just can’t assess it. If you truly have patient best interest at heart, it is a no brainer.
But guess who is most vocally opposed to MOTA? The for-profit Methadone clinics who, coincidentally, stand to lose the most money if MOTA passes. Disguised under a group called “The American Association for the Treatment of Opioid Dependence,” these for-profit clinics have put out several statements- written by non-physicians-claiming outpatient physician specialist prescribing of methadone would be “dangerous.” Pure baloney. It’s only dangerous for their pocketbooks. This is like Coca-Cola claiming its dangerous to drink Pepsi. More medication treatment choices for patients potentially means less patients and less profits for them. They largely base this self-serving claim on studies looking at outpatient methadone prescriptions written by all types of providers (non-specialists). In contrast, the MOTA act specifies that only board-certified addiction psychiatrists would be able to prescribe and monitor outpatient methadone. These physician specialists have the highest level of training and expertise on Addiction treatment than any other medical professional. Most current methadone clinic providers are not Addiction Psychiatrists or Addiction Medicine Physicians. MOTA would increase access to life-saving medication while raising the existing training and specialty requirements for who can dispense it. Don’t be fooled by Coca-Cola telling you not to buy Pepsi. We need to look beyond money and do what is best for the patient, not our pocketbook: we need to pass MOTA.
1.White House/Congress: Provide Federal Funding to Existing Harm Reduction Initiatives
Some patients are just not ready to stop using drugs. Or can’t. The number one risk factor for fatal overdose is using alone. If folks aren’t ready to stop, we can still save lives by making drug use less deadly. The Never Use Alone Line and the Massachusetts Overdose Prevention Helpline are two Overdose Prevention Lifelines that people can call when they are going to use drugs. These lines are manned by volunteers who simply stay on the phone while the person uses their substance of choice to make sure they don’t die. If they become unresponsive, the volunteer calls 911. In the past year alone, Stephen Murray (founder) and other folks at The Massachusetts Overdose Prevention Helpline have prevented 11 near fatal overdoses! While both phone numbers can be used by any caller in the country, right now both phone numbers have no federal funding source. They operate with a group of largely unpaid good Samaritans who donate their time freely to prevent people from dying. Even on a small scale, these initiatives are saving roughly one life per month through volunteers alone. Imagine what we could do with greater awareness of these resources and more people manning the lines? Both things require money.
Some folks will grumble, saying, “We shouldn’t spend taxpayer money to encourage drug use.” The auto industry also complained when the national seat belt law was passed in 1968. They claimed that requiring seat belts would encourage people to speed. Since that time, approximately 374, 276 lives have been saved due to seat belts. Rates of speeding did not rise accordingly.
Change is hard. At the same time, the world is run by people who show up and speak out. Showing up in any way you can to support simple, common-sense solutions to the Opioid Epidemic will save lives. Whether that means advocating on Capitol Hill for MOTA, spreading the word about overdose prevention lines, or simply reposting and sharing this article with others, every little bit helps. With just a little energy, passion, and conviction, we can stop the opioid epidemic- one jumbo jet at a time